Disc Replacement and Spine Fusion Surgeries
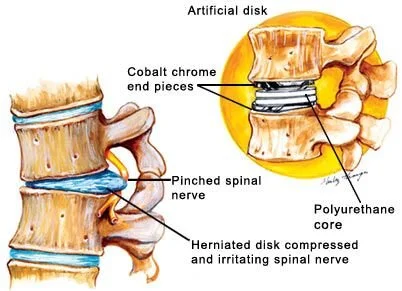
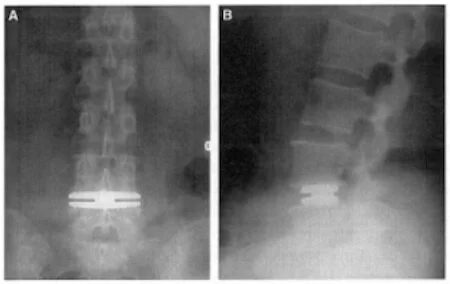
Lumbar Total Disc Arthroplasty/ Disc Replacement
When is it done?
18-60 years with severe chronic pain with inability to perform daily activities from a single degenerative disc ( as seen on recent tests, with no significant facet joint disease at that level) for atleast 1 year
AND Absence of unmanaged significant behavioral health disorders (e.g. major depressive disorder, chronic pain syndrome, psychiatric conditions, drug and alcohol abuse, general pain disorders), fibromyalgia
AND having regular follow up medical appointments with prescription strength medicines and exercises program for 6 months continuously
Lumbar Spine Fusion with or without Decompression:
Uninstrumented fusion (with bone graft only, no hardware/ screws/ plates) may be preferred, as it has fewer subsequent complications. Larger instrumented (PLIF, TLIF, etc.) fusion techniques should be used only for significant instability of the spine as seen on imaging tests.
Urgent:
Infection, tumor, severe or worsening weakness, inability to control urine or stool, unable to feel in the saddle area, bleeding, fractures/ dislocations
Non urgent :
Pain, pain on walking, or leg pain that significantly affects daily function and activities for atleast 6 months
AND your tests show results that correspond to your symptoms
AND your exam shows nerve exam problems or special test abnormalities
AND you tried atleast 2 of medicines, exercise program, spine injections for atleast 6 weeks with no/ minimal benefit
AND unstable spine, or vertebrae slipping one each other (severe or progressive), or if failed previous surgeries with signifiant function improvement expected or after 6-12 months of behavior therapy and exercises if there is no nerve pinching but severe spine degeneration
Spine surgeries should not be done when:
weak bones (osteoporosis); infection, severe heart or lung problems, low red blood cells (anemia), malnutrition
other muscles, joints, peripheral nerves or psychiatric issues causing the pain
smoking 6 weeks before or during the surgery healing process
when obesity is thought to increase chances of complications, delayed healing after surgery, or prevents following through with rehabilitation exercises after surgery
Caution:
Lumbar spine fusion is an extensive surgery and the healing process takes a long time (about 3 to 6 months, and up to 18 months)
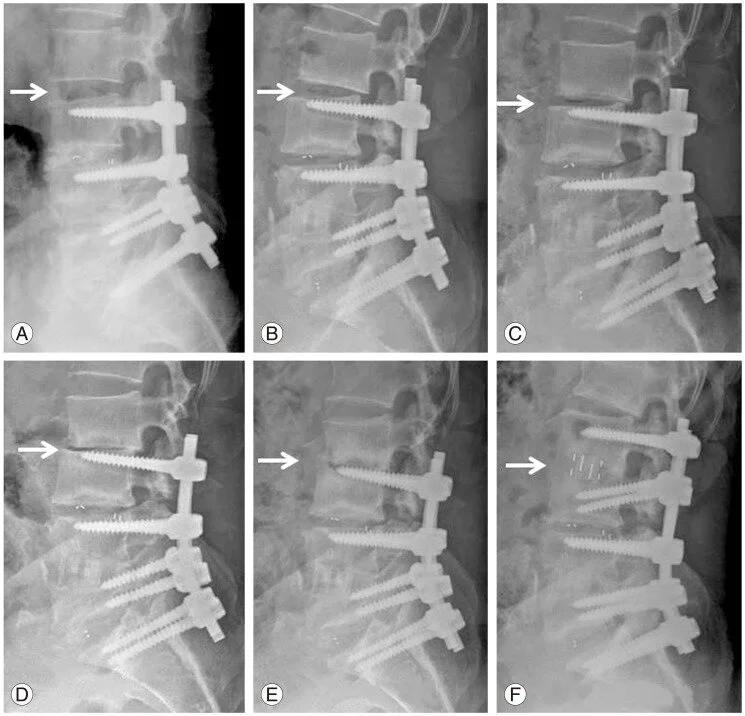
The spine fusion forever changes the biomechanics of the back and is thought to increase the stress placed on the other (non-fused) joints in the lower spine. This leads to accelerated degeneration of the adjacent levels of the spine, including instability. In one study, more than one-third of patients required surgery at an adjacent level by 10 years.
This is more prominent when back of the vertebrae is removed or fused.
Some operative techniques proposed to address this problem including posterior motion preserving and dynamic stabilization techniques, showed low to insufficient evidence that these techniques are superior in preventing adjacent segment disease long term.
A, B, C, D, E show progressive fastened degeneration of the adjacent disc space above the fusion surgery, until it also eventually needed fusion in F. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4591457/
Other Complications:
Include instrumentation failure, bone graft donor, site pain, superficial infection, deep wound infection, and graft extrusion
There is an increased likelihood of complications with instrumented fusion (as opposed to just using one’s own bone graft), although the majority of them are minor.
There is some evidence that morbid obesity increases hospital length of stay, mortality and postoperative complications of spinal fusion surgery and results in increases in cost.
What kind of surgery is better?
Lumbar laminectomy alone has been shown to be better for patients with lumbar stenosis in the absence of instability.
Lumbar decompression and fusion have been better in patients with spondylolisthesis (vertebrae slipping slightly over each other). Fusion best when there is spondylolisthesis only. Fusion has 17% increase in reoperative risk and nearly twice the risk of complications relative to decompression-alone.
Lumbar discectomy (removal of disc) and fusion can also be done following failed lumbar disc arthroplasty implant
Sacroiliac joint Fusion:
Minimally invasive sacroiliac joint fusion is standard, unless there were prior surgeries, fractures/ spine deformity, infection or tumor.
For buttock/ sacroiliac pian and for all the same indications/ reasons as for above lumbar fusion. Similar complications apply. In addition these are needed:
Sacroiliac joint injections showed significant pain relief
AND had 6 months of combination treatment with medicines, exercises,
AND no other muscles, peripheral nerves, lumbar spine, other joint or psychiatric issues causing the pain
AND Absence of unmanaged significant behavioral health disorders (e.g. major depressive disorder, chronic pain syndrome, psychiatric conditions, drug and alcohol abuse, general pain disorders)
AND non smoking for 6 weeks before, during and after surgery
What else can we add or work on? Please let us know in the comments. No need to log in…